Table of Contents
Toggle
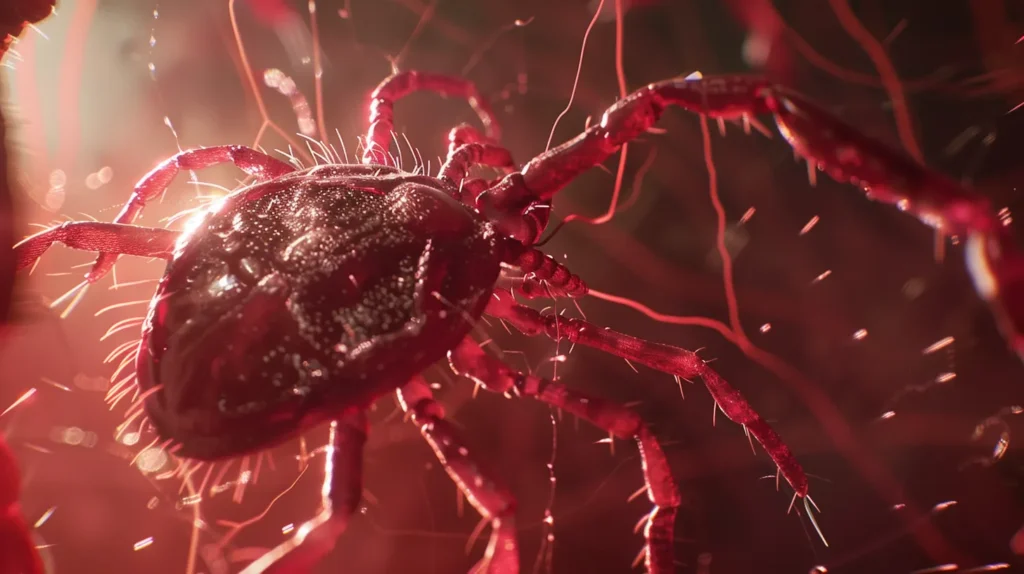
Understanding Lyme Disease: Symptoms, Diagnosis, Treatment, and Prevention
Lyme disease affects thousands of people each year, yet many remain unaware of its risks and symptoms. This article will guide you through the essential aspects of Lyme disease, including its symptoms, diagnosis, and treatment options. By understanding these key points, you’ll be better equipped to protect yourself and your loved ones from this tick-borne illness. Learn how to recognize early signs, seek proper medical care, and implement effective prevention strategies to reduce your risk of contracting Lyme disease.
Key Takeaways
- Lyme disease is transmitted by tick bites and primarily occurs in North America and Europe
- Early symptoms include a distinctive bull’s-eye rash and flu-like symptoms
- Diagnosis involves laboratory tests and careful consideration of patient history and symptoms
- Standard antibiotic treatments are effective, especially when started early
- Prevention strategies include using tick repellents, wearing protective clothing, and conducting regular tick checks
What Is Lyme Disease?

Lyme disease is a bacterial infection transmitted to humans through tick bites. This zoonosis, recognized by the American Academy of Family Medicine, primarily occurs in North America and Europe, including the United Kingdom. The disease is caused by Borrelia burgdorferi bacteria and can lead to various symptoms, including mental health issues, if left untreated. Understanding the bacteria, geographic distribution, and transmission methods is crucial for prevention and timely treatment with appropriate medicines.
Understanding the Bacteria Behind Lyme Disease
Borrelia burgdorferi, the bacteria responsible for Lyme disease, belongs to the spirochete family. These spiral-shaped microorganisms thrive in ticks, particularly those of the Ixodes ricinus species, which act as vectors for transmission to humans. The bacteria’s ability to adapt to different climates contributes to its widespread distribution across North America and Europe.
Once transmitted to humans through a tick bite, B. burgdorferi can cause various symptoms, including fever and a characteristic rash known as erythema migrans. This rash often appears as a bullseye pattern and may be accompanied by flu-like symptoms. If left untreated, the infection can progress, potentially leading to more severe complications such as arthritis, neurological issues, and dermatitis.
Common Geographic Locations for Lyme Disease
Lyme disease predominantly occurs in specific regions of North America and Europe. In the United States, the highest incidence rates are found in the Northeast, Mid-Atlantic, and Upper Midwest regions, where ticks carrying Borrelia burgdorferi are most prevalent. Primary care physicians in these areas often encounter patients with symptoms requiring further investigation, including neuroimaging and ELISA tests.
European countries such as Germany, Austria, and Sweden also report significant cases of Lyme disease. Health care providers in these regions must remain vigilant, as the disease’s geographic distribution continues to expand due to climate change and alterations in land use patterns. This expansion emphasizes the need for ongoing research and experiments to improve diagnostic methods and treatment protocols across affected areas.
Transmission Methods of Lyme Disease
Lyme disease is primarily transmitted through the bite of infected Ixodes ricinus ticks. These ticks attach to humans and feed on their blood, potentially transmitting Borrelia burgdorferi bacteria. The Mayo Clinic reports that ticks must generally be attached for 36 to 48 hours to transmit the bacteria effectively.
While tick bites are the main transmission method, emergency medicine professionals also encounter cases in emergency departments where patients present with neck stiffness and other symptoms. It’s important to note that Lyme disease cannot be transmitted from person to person through physical contact, sharing food, or other means. The following table illustrates the transmission process:
| Stage | Description |
|---|---|
| 1. Tick Attachment | Infected tick attaches to human skin |
| 2. Feeding Period | Tick feeds on blood for 36-48 hours |
| 3. Bacterial Transmission | Borrelia burgdorferi enters bloodstream |
| 4. Infection Onset | Symptoms may appear within days or weeks |
Recognizing Lyme Disease Symptoms

Recognizing Lyme disease symptoms is crucial for early diagnosis and treatment. Early signs include flu-like symptoms and a distinctive rash. Chronic Lyme disease can manifest with more severe symptoms, potentially leading to long-term complications. Understanding these symptoms, from initial onset to potential allergic reactions and the need for antibiotic prophylaxis, is essential for proper management. Immunology plays a key role in the body’s response to the infection, which can affect various body parts, including the elbow.
Early Signs of Lyme Disease
Early signs of Lyme disease typically appear within 3 to 30 days after an infected tick bite. The most recognizable symptom is erythema migrans, a red circular rash that often resembles a bull’s-eye pattern and expands gradually. This rash occurs in approximately 70-80% of infected individuals and may be accompanied by flu-like symptoms such as fever, chills, fatigue, and body aches.
In some cases, early Lyme disease can present without the characteristic rash, making diagnosis challenging. Patients may experience headaches, neck stiffness, and swollen lymph nodes. Serological tests may not be reliable in the early stages, as antibodies take time to develop. Healthcare providers often rely on clinical presentation and potential exposure to ticks, particularly nymphs, which are responsible for most Lyme disease transmissions to humans and other mammals.
Distinctive Characteristics of Lyme Disease Rash
The distinctive Lyme disease rash, known as erythema migrans, typically appears at the site of the tick bite within 3 to 30 days. This rash, often described as a “bull’s-eye” pattern, begins as a small red spot that gradually expands over days, potentially reaching up to 12 inches in diameter. Internal medicine specialists note that the rash may feel warm to the touch but is usually not painful or itchy.
While the classic bull’s-eye appearance is characteristic, patients may present with variations in rash appearance. Some rashes may be uniformly red or have a bluish hue at the center. Ixodes ticks, particularly the nymphal stage, are primarily responsible for transmitting Borrelia burgdorferi, the bacteria causing Lyme disease. It’s important to differentiate this rash from those caused by other tick-borne illnesses such as anaplasmosis or bites from Dermacentor variabilis ticks. The following table illustrates key characteristics of the Lyme disease rash:
| Characteristic | Description |
|---|---|
| Shape | Circular or oval, often with central clearing |
| Size | Expands gradually, up to 12 inches |
| Color | Red, sometimes with bluish center |
| Sensation | Warm, usually not painful or itchy |
| Duration | Persists for several weeks if untreated |
Symptoms of Chronic Lyme Disease
Chronic Lyme disease, characterized by persistent symptoms lasting months or years, can affect various parts of the body, including the central nervous system. Patients may experience neurological issues, such as memory problems, difficulty concentrating, and mood changes. The host’s immune response to Borrelia burgdorferi, transmitted by Ixodes pacificus ticks, can lead to ongoing inflammation and tissue damage.
Treatment for chronic Lyme disease often involves long-term use of antibiotics and other medications to manage symptoms. However, the medical community debates the existence of chronic Lyme disease, as evidence supporting its diagnosis and treatment remains controversial. Patients with persistent symptoms should consult healthcare providers specializing in tick-borne illnesses for comprehensive evaluation and personalized treatment plans.
Complications and Long-Term Effects
Long-term complications of Lyme disease can arise if the infection goes untreated or is not adequately managed. Patients may experience persistent joint pain, neurological issues, and cardiac problems. The western blot test, developed by Willy Burgdorfer, helps confirm Lyme disease diagnosis in later stages when symptoms become more complex.
Prevention remains crucial for reducing the risk of long-term effects. Using insect repellent and proper tick checks can significantly decrease the chances of contracting Lyme disease. Studies have shown varying efficacy rates for different prevention methods, emphasizing the importance of a comprehensive approach to protect against tick bites and potential complications.
Confirming a Lyme Disease Diagnosis

Confirming a Lyme disease diagnosis involves specific laboratory tests and careful consideration of patient history. Dermatology plays a role in identifying characteristic rashes. Differentiating Lyme disease from other conditions is crucial, as symptoms can mimic autoimmune disorders. Accurate diagnosis guides appropriate treatment, which may include cephalosporin antibiotics. In complex cases, synovectomy may be considered for joint involvement. Understanding the Borrelia burgdorferi sensu lato complex is essential for comprehensive diagnosis and management.
Laboratory Tests Used for Diagnosis
Laboratory tests play a crucial role in diagnosing Lyme disease, especially when symptoms like palpitations or facial muscle weakness are present. The European Centre for Disease Prevention and Control recommends a two-tiered testing approach, starting with an enzyme-linked immunosorbent assay (ELISA) followed by a Western blot test if the ELISA is positive or equivocal.
These tests detect antibodies against Borrelia burgdorferi, the bacteria causing Lyme disease. However, false negatives can occur in early stages, and false positives may result from conditions like rheumatoid arthritis. Therefore, laboratory results must be interpreted in conjunction with clinical symptoms and exposure history for accurate diagnosis.
Importance of Patient History
Patient history plays a crucial role in diagnosing Lyme disease, especially when symptoms like syncope occur. Healthcare providers at institutions such as Johns Hopkins emphasize the importance of detailed patient interviews to identify potential tick exposures and early symptoms. This information helps differentiate Lyme disease from other conditions like spotted fever, particularly in areas where Ixodes persulcatus ticks are prevalent.
A thorough patient history also guides the selection of appropriate diagnostic tests, including enzyme-based assays. Clinicians consider factors such as recent outdoor activities, travel to endemic areas, and the presence of characteristic rashes or flu-like symptoms. This comprehensive approach enhances diagnostic accuracy and informs treatment decisions, especially when laboratory results are inconclusive.
Differentiating Lyme Disease From Other Conditions
Differentiating Lyme disease from other conditions requires careful consideration of symptoms and diagnostic tests. Healthcare providers must distinguish Lyme disease from illnesses like Rocky Mountain spotted fever, which can present similar symptoms. Pathogen transmission methods and affected body parts, such as the foot, can provide important clues for accurate diagnosis.
Laboratory tests, including those measuring immunoglobulin G levels, help differentiate Lyme disease from other infections. Healthcare providers consider factors like breastfeeding status when interpreting test results and recommending treatment options. Accurate differentiation ensures appropriate care and prevents unnecessary antibiotic use.
Exploring Treatment Options for Lyme Disease

Treatment options for Lyme disease encompass standard antibiotic regimens and alternative approaches, addressing both acute and persistent symptoms. Health care providers consider factors such as the presence of co-infections like babesia when developing treatment plans. As a notifiable disease, proper management is crucial to prevent complications affecting the skin, nerves, and other body systems. This section explores evidence-based treatments and ongoing research in Lyme disease care.
Standard Antibiotic Treatments
Standard antibiotic treatments for Lyme disease target the bacteria Borrelia burgdorferi, which can affect the peripheral nervous system. Doxycycline is the primary antibiotic used for most cases, while alternatives like cefuroxime axetil or cefotaxime may be prescribed for patients with specific contraindications. These treatments aim to eliminate the infection before it spreads to other body systems, unlike mosquito-borne diseases that require different approaches.
The duration and dosage of antibiotic treatment depend on the stage and severity of Lyme disease. Early-stage infections typically require a 10 to 14-day course, while more advanced cases may need longer treatment periods. Healthcare providers must consider potential side effects and drug interactions when prescribing antibiotics, as well as educate patients on proper administration. For example, patients should avoid applying nail polish during treatment to monitor for potential skin reactions.
The following table illustrates standard antibiotic treatments for Lyme disease:
| Antibiotic | Typical Duration | Common Usage |
|---|---|---|
| Doxycycline | 10-21 days | First-line treatment for most cases |
| Amoxicillin | 14-21 days | Alternative for pregnant women and young children |
| Cefuroxime axetil | 14-21 days | Alternative for patients allergic to penicillin |
| Cefotaxime | 14-28 days | Intravenous treatment for severe cases |
Alternative Approaches and Controversies
Alternative approaches to treating Lyme disease have emerged, sparking controversy within the medical community. Some practitioners advocate for prolonged antibiotic therapy, claiming it addresses persistent symptoms better than standard treatments. However, the Food and Drug Administration cautions against these extended regimens due to potential risks and lack of proven efficacy through polymerase chain reaction testing.
Debate continues regarding the role of Ixodes scapularis ticks in transmitting multiple pathogens and the implications for treatment. Researchers explore novel therapies targeting specific antigens of Borrelia burgdorferi, aiming to develop more effective treatments. These ongoing studies may provide new insights into managing Lyme disease and its associated long-term effects.
Addressing Persistent Symptoms
Addressing persistent symptoms in Lyme disease patients involves a comprehensive approach, including physical examination and targeted interventions. Healthcare providers in North America, particularly in the northeastern United States, encounter cases of lingering symptoms such as fatigue, joint pain, and cognitive issues. Edema, a common manifestation, requires careful assessment and management to improve patient comfort and mobility.
Treatment strategies for persistent symptoms may include a combination of antibiotics, anti-inflammatory medications, and supportive therapies. Healthcare professionals must consider the possibility of co-infections transmitted by the same insect vector, as these can complicate the clinical picture and require additional interventions. The following table outlines common persistent symptoms and their management approaches:
| Persistent Symptom | Management Approach |
|---|---|
| Fatigue | Graded exercise therapy, sleep hygiene |
| Joint pain | Physical therapy, anti-inflammatory medications |
| Cognitive issues | Cognitive rehabilitation, neuropsychological evaluation |
| Edema | Compression therapy, lymphatic drainage |
Implementing Effective Lyme Disease Prevention Strategies

Effective Lyme disease prevention strategies are crucial for reducing incidence rates. Best practices for tick avoidance, protective clothing, and tick repellents like permethrin play key roles in prevention. Regular tick checks are essential for early detection. Disease surveillance methods with high sensitivity and specificity help monitor and control Lyme disease spread, emphasizing the importance of comprehensive prevention approaches.
Best Practices for Tick Avoidance
The Infectious Diseases Society of America recommends several best practices for tick avoidance to prevent Lyme disease. These include using EPA-registered insect repellents containing DEET, picaridin, or IR3535 when outdoors in tick-prone areas. Additionally, treating clothing and gear with products containing 0.5% permethrin can effectively repel ticks for several washes.
The Centers for Disease Control and Prevention advises walking in the center of trails and avoiding areas with tall grass and leaf litter where ticks are common. After outdoor activities, individuals should conduct thorough tick checks, paying special attention to areas such as the armpits, groin, and scalp. Early tick removal can significantly reduce the risk of Lyme disease transmission and associated symptoms like lymphadenopathy or shortness of breath.
Protective Clothing and Tick Repellents
Protective clothing plays a crucial role in preventing tick bites and reducing the risk of Lyme disease and other tick-borne illnesses like Borrelia miyamotoi infection. Individuals should wear long-sleeved shirts and pants tucked into socks when venturing into tick-prone areas, such as wooded regions in Minnesota or Poland. Light-colored clothing helps spot ticks more easily, allowing for prompt removal before they can transmit pathogens.
Effective tick repellents contain active ingredients like DEET, picaridin, or permethrin. These products, when applied correctly, significantly reduce the chance of tick attachment and potential transmission of disseminated disease. Healthcare providers recommend reapplying repellents according to manufacturer instructions, especially in high-risk areas where tick-borne illnesses, including those causing pericarditis, are prevalent.
Importance of Regular Tick Checks
Regular tick checks are crucial for preventing Lyme disease transmission, as recommended by the American Academy of Pediatrics and disease control experts. Research shows that prompt removal of ticks within 24 hours significantly reduces the risk of infection. Individuals should thoroughly examine their skin, paying special attention to areas where ticks commonly attach, such as the scalp, armpits, and groin.
Deer ticks, the primary vectors for Lyme disease, can be as small as a poppy seed, making careful inspection essential. After outdoor activities in tick-prone areas, individuals should conduct a full-body check and examine clothing and gear for any attached ticks. Proper removal techniques, such as using fine-tipped tweezers to grasp the tick close to the skin’s surface, help prevent leaving tick mouthparts in the tissue. The following table outlines key steps for effective tick checks:
| Step | Action |
|---|---|
| 1 | Conduct full-body inspection |
| 2 | Check clothing and gear |
| 3 | Use fine-tipped tweezers for removal |
| 4 | Clean bite area with antiseptic |
| 5 | Monitor for symptoms |
Understanding the Curability of Lyme Disease

Lyme disease curability depends on various factors, including early detection and appropriate treatment. Success rates of treatment protocols vary, with early intervention typically yielding better outcomes. Factors such as mouse reservoirs, fatigue severity, and involvement of cranial nerves can influence recovery. Understanding these aspects is crucial for managing Lyme disease effectively and preventing complications like increased intracranial pressure.
Factors Influencing Recovery
Recovery from Lyme disease depends on several factors, including the timing of antibiotic treatment initiation and the extent of infection. Early intervention, before the bacteria spreads to the spinal cord and other organs, typically leads to better outcomes. The type and duration of antibiotic therapy also play crucial roles in recovery, with healthcare providers adjusting treatment based on the patient’s response and potential side effects.
The patient’s overall health and immune function influence recovery rates. Individuals with robust immune systems may clear the infection more effectively, while those with compromised immunity might face prolonged recovery periods. Regular exercise and physical therapy can aid in managing symptoms and improving joint function, particularly when synovial fluid is affected. Healthcare providers often recommend a balanced approach to activity and rest to support the healing process.
Success Rates of Treatment Protocols
Treatment protocols for Lyme disease have shown varying success rates, depending on factors such as the stage of infection and the patient’s overall health. Early intervention with appropriate antibiotics has demonstrated high success rates, particularly when initiated before the Borrelia burgdorferi bacteria spreads beyond the initial infection site. Microbiology studies have revealed that targeting the spirochete in its larval stage can significantly improve treatment outcomes.
The success of treatment protocols can be influenced by the ecology of tick habitats and the prevalence of infected vectors. Healthcare providers may use electrocardiography to monitor potential cardiac complications during treatment. Some patients have reported benefits from incorporating lemon-based remedies as complementary therapies, although scientific evidence supporting their efficacy remains limited. The following factors contribute to the success rates of Lyme disease treatment protocols:
- Timing of antibiotic initiation
- Appropriate antibiotic selection
- Patient compliance with treatment regimens
- Presence of co-infections
- Individual immune response
Debunking Common Lyme Disease Myths

Common misconceptions about Lyme disease symptoms, treatments, and geographic distribution often lead to confusion. This section addresses myths surrounding symptoms like lightheadedness and mouth issues, explores treatment misconceptions, and clarifies geographic myths, including prevalence in New Jersey. Understanding these facts helps distinguish Lyme disease from conditions like ALS and encephalopathy, ensuring accurate diagnosis and appropriate care.
Misconceptions About Lyme Disease Symptoms
Many misconceptions surround Lyme disease symptoms, leading to potential misdiagnosis. Contrary to popular belief, not all patients develop the characteristic bull’s-eye rash, and symptoms can vary widely. The American Academy of Neurology emphasizes that neurological symptoms, such as brain fog and cognitive issues, may occur without the presence of obvious physical signs, making early detection challenging.
Another common misconception is that Lyme disease always causes immediate, severe symptoms. In reality, the Borrelia spirochaete can remain dormant in the body for extended periods, causing delayed onset of symptoms. While some patients experience intense itching, this is not a universal symptom and should not be relied upon for diagnosis. Understanding these variations in symptom presentation is crucial for healthcare providers to accurately identify and treat Lyme disease cases.
Myths Surrounding Treatments and Cures
Misconceptions about Lyme disease treatments can lead to ineffective or potentially harmful practices. While some believe that long-term antibiotic therapy is necessary for all cases, data shows that standard short-term treatments are often sufficient. Penicillin and other appropriate antibiotics, when administered early, can effectively treat the infection without resorting to prolonged regimens.
Another myth surrounding Lyme disease treatment involves the use of alternative therapies for pets and humans alike. While some claim that certain skin applications or herbal remedies can cure the disease, scientific evidence does not support these assertions. Healthcare providers emphasize the importance of evidence-based treatments and caution against unproven cures that may delay proper medical intervention.
Clarifying Geographic Myths
Geographic myths surrounding Lyme disease often lead to misconceptions about its prevalence and risk. While many associate Lyme disease primarily with the northeastern United States, epidemiological studies show that it occurs in various regions worldwide. The species of ticks carrying Borrelia burgdorferi, the bacteria causing Lyme disease, have expanded their habitats due to climate change and altered land use patterns, leading to increased cases in previously low-risk areas.
Another common geographic myth is that Lyme disease only affects rural populations. However, urban and suburban areas with parks and green spaces can also harbor infected ticks. This misconception can delay diagnosis and treatment, potentially leading to complications such as carditis or chronic inflammation. Healthcare providers stress the importance of considering Lyme disease as a possibility regardless of a patient’s geographic location, especially when symptoms and exposure history align. Protein A testing can aid in diagnosis across diverse geographic regions.
Key points about Lyme disease geographic distribution:
- Occurs in multiple regions globally, not just northeastern US
- Tick habitats expanding due to climate change
- Urban and suburban areas can also pose risks
- Consider Lyme disease regardless of patient location
- Protein A testing aids diagnosis across regions
Why Awareness and Education Matter
Awareness and education about Lyme disease are crucial for effective prevention and management. Understanding its impact on communities helps prioritize public health measures. Resources for further learning equip individuals with knowledge to recognize symptoms like relapsing fever and hair loss. Regular medical check-ups enable early detection and treatment with antibiotics like amoxicillin, preventing complications such as increased pressure or tick paralysis.
Understanding Lyme Disease's Impact on Communities
Lyme disease significantly impacts communities, affecting public health and economic resources. In Canada, where Lyme disease is prevalent, communities face challenges in educating residents about proper tick removal techniques using tweezers and recognizing early symptoms like neck stiffness and muscle pain. Public health initiatives focus on raising awareness to prevent complications such as myocarditis, a potential cardiac manifestation of Lyme disease.
The impact of Lyme disease extends beyond individual health, affecting community productivity and healthcare systems. Local health departments in endemic areas invest resources in surveillance, education, and prevention programs. These efforts aim to reduce the incidence of Lyme disease and its associated complications, ultimately improving community health outcomes. The following table illustrates the multifaceted impact of Lyme disease on communities:
| Impact Area | Description |
|---|---|
| Public Health | Increased burden on healthcare systems |
| Economic | Lost productivity and medical costs |
| Education | Resources allocated for awareness programs |
| Recreation | Changes in outdoor activity patterns |
| Environmental Management | Efforts to control tick populations |
Resources for Further Learning
Numerous resources are available for further learning about Lyme disease, including educational materials from reputable health organizations. These resources provide comprehensive information on symptoms such as joint effusion and headaches, as well as prevention strategies like using sunscreen to reduce tick exposure during outdoor activities. Online courses and webinars offer in-depth knowledge on Lyme disease diagnosis, treatment options, and long-term health implications.
Local health departments and community centers often host informational sessions on Lyme disease awareness, focusing on behavior modifications to reduce tick encounters. These programs may include hands-on demonstrations of proper tick removal techniques and discussions on recognizing early symptoms. Additionally, support groups for individuals affected by Lyme disease provide valuable insights into managing the condition and navigating treatment options.
Encouraging Regular Medical Check-Ups
Regular medical check-ups play a crucial role in the early detection and management of Lyme disease, particularly in regions of Europe where the disease is prevalent. Physicians can monitor patients’ heart rate and overall physical health, identifying potential symptoms before they progress. These check-ups allow healthcare providers to assess risk factors based on patients’ habitats and outdoor activities, providing tailored preventive advice.
Encouraging individuals to schedule routine medical examinations can significantly improve Lyme disease outcomes. During these visits, doctors can perform thorough physical assessments, addressing any concerns about tick exposure or unusual symptoms. Regular check-ups also provide opportunities for healthcare professionals to educate patients about Lyme disease prevention strategies, fostering a proactive approach to maintaining health in tick-prone environments.
Frequently Asked Questions
What is Lyme disease?
Lyme disease is a tick-borne bacterial infection caused by Borrelia burgdorferi. It typically begins with a characteristic bull’s-eye rash and can progress to cause flu-like symptoms, joint pain, and neurological issues if left untreated. Early antibiotic treatment is crucial for effective management.
What are the causes of Lyme disease?
Lyme disease is primarily caused by the bacterium Borrelia burgdorferi, transmitted to humans through the bite of infected blacklegged ticks. These ticks typically become infected after feeding on mice or deer carrying the bacteria. Outdoor activities in wooded or grassy areas increase the risk of exposure.
What are the symptoms of Lyme disease?
Early symptoms of Lyme disease often include fever, chills, fatigue, body aches, headache, and a distinctive bull’s-eye rash called erythema migrans. If left untreated, later stages may involve joint pain, neurological problems, and heart issues.
How is Lyme disease diagnosed?
Lyme disease diagnosis involves a combination of clinical evaluation, patient history, and laboratory tests. Doctors assess symptoms, look for the characteristic bulls-eye rash, and consider potential tick exposure. Blood tests detecting antibodies against Borrelia burgdorferi, the bacteria causing Lyme disease, are often used to confirm the diagnosis.
What are the common Lyme disease treatments?
Common Lyme disease treatments include antibiotics like doxycycline, amoxicillin, or cefuroxime. These are typically prescribed for 2-4 weeks, depending on the stage of infection. In severe cases, intravenous antibiotics may be necessary. Symptom management and supportive care are also important components of treatment.
Can Lyme disease be cured completely?
Lyme disease can be effectively treated with antibiotics, especially when caught early. However, complete cure may be challenging in some cases, as symptoms can persist even after treatment. Long-term management and support are often necessary for individuals with chronic Lyme disease.
Can pets get Lyme disease?
Yes, pets can get Lyme disease. Dogs are particularly susceptible, while cats rarely contract it. Transmitted by infected ticks, Lyme disease in pets can cause fever, lameness, and joint swelling. Regular tick prevention and prompt removal are key to protecting pets from this illness.
Can you get Lyme disease more than once?
Yes, you can get Lyme disease more than once. Reinfection is possible if you’re bitten by another infected tick, as previous infection doesn’t guarantee immunity. Each new exposure carries the risk of contracting the disease, making ongoing tick prevention crucial for those in endemic areas.
Conclusion
Understanding Lyme disease is crucial for effective prevention, early diagnosis, and timely treatment. Recognizing symptoms, from the characteristic bull’s-eye rash to neurological issues, enables prompt medical intervention and improved outcomes. Implementing preventive measures, such as tick avoidance strategies and regular tick checks, significantly reduces the risk of infection. Ongoing education and awareness about Lyme disease empower individuals and communities to protect their health and manage this complex illness effectively.

Dr. Emily Smith is a dedicated and experienced general practitioner with a focus on treating both chronic and acute medical conditions. With a comprehensive medical background, she provides personalized and compassionate care to her patients. Dr. Smith has a deep understanding of a wide range of medical issues and is committed to helping individuals manage their health effectively.
